Blood-Brain Barrier Disruption Implicated in Post-traumatic Epilepsy
Blood-Brain Barrier Disruption Implicated in Post-traumatic Epilepsy
October 31, 2008
There is a high occurrence of prolonged and lasting breakdown of the blood-brain barrier after mild traumatic brain injury, especially among patients who develop epilepsy, according to findings reported in the July issue of the Journal of Neurology, Neurosurgery, and Psychiatry.
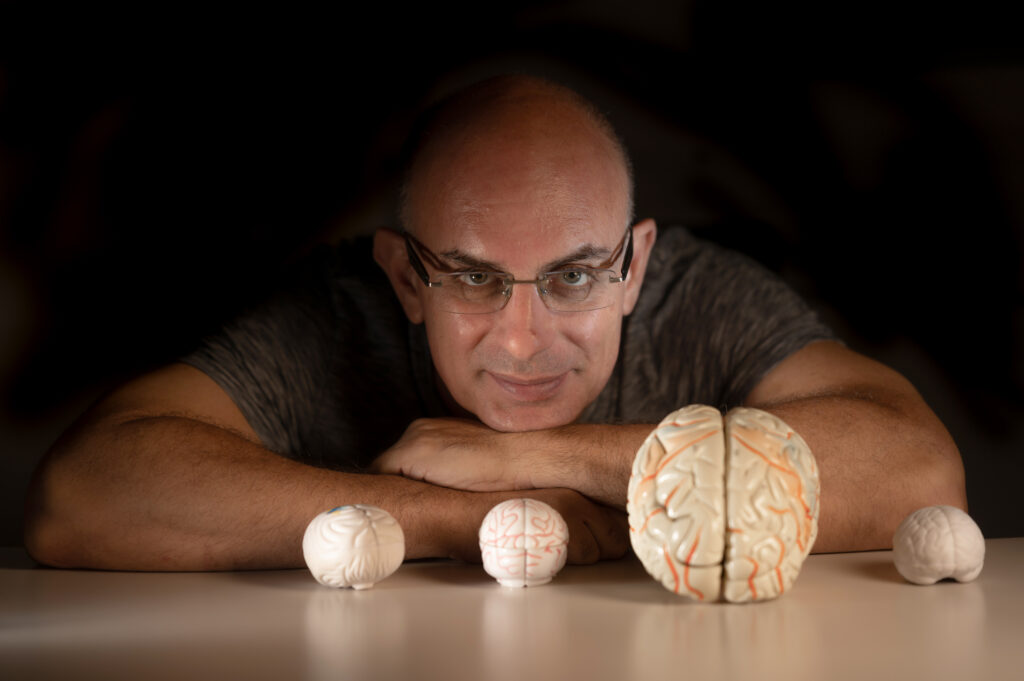
“Post-traumatic epilepsy occurs in 20% to 40% of patients after head injury and is often difficult to treat,” Dr. Alon Friedman told Reuters Health. “However, at present, there are no means to predict who will develop epilepsy and no measures for its prevention,” he explained.
Dr. Friedman, of Ben-Gurion University of the Negev, Beer-Sheva, Israel, and his colleagues have shown in recent animal experiments that “opening the blood-brain barrier (BBB) leads to network changes, long-lasting epileptiform activity and eventual neurodegeneration.”
In the current study, the researchers examined the frequency and extent of increased BBB permeability in 32 head trauma patients, of whom 17 had post-traumatic epilepsy (PTE).
Spectral EEG analyses showed significant slowing in patients with traumatic brain injury but no significant differences were observed between patients with epilepsy and those without.
Patients with PTE were significantly more likely to have a lesion on their MRI scans than those without epilepsy (80% versus 30.8%), but there was no significant difference in the size of the lesion between the groups.
Overall, 76.9% of patients with PTE had BBB disruption, compared with 33.3% of patients without epilepsy (p = 0.047). Increased BBB permeability could be observed months or years following the trauma.
In 70% of patients with BBB disruption, the source of abnormal delta band activity could be localized to the area of the BBB disruption.
“The research (together with our animal studies) predicts that patients with prolonged BBB breakdown after brain injury are at greater risk to develop epilepsy,” Dr. Friedman said. “Our results offer new diagnostic tools with potential preventive therapeutic implications,” he noted.
Dr. Friedman and his colleagues are currently conducting a prospective study in which they are closely following patients immediately after head trauma using MRI and EEG.
“This study will challenge our hypothesis that prolonged BBB breakdown predicts the development of epileptic seizures,” the researcher said.
“We also continue our basic research for better understanding the mechanisms underlying brain dysfunction under BBB breakdown and testing new therapeutic strategies to prevent the development of epilepsy.”