Coronavirus Test Shortages Trigger a New Strategy
Coronavirus Test Shortages Trigger a New Strategy
May 13, 2020
Scientific American — Unless there is widespread testing for COVID-19, experts warn, cases will surge as governments reopen more businesses and public spaces.
But there is still a woeful shortage of diagnostic tests for coronavirus infections, because of unprecedented demand for chemicals and supplies.
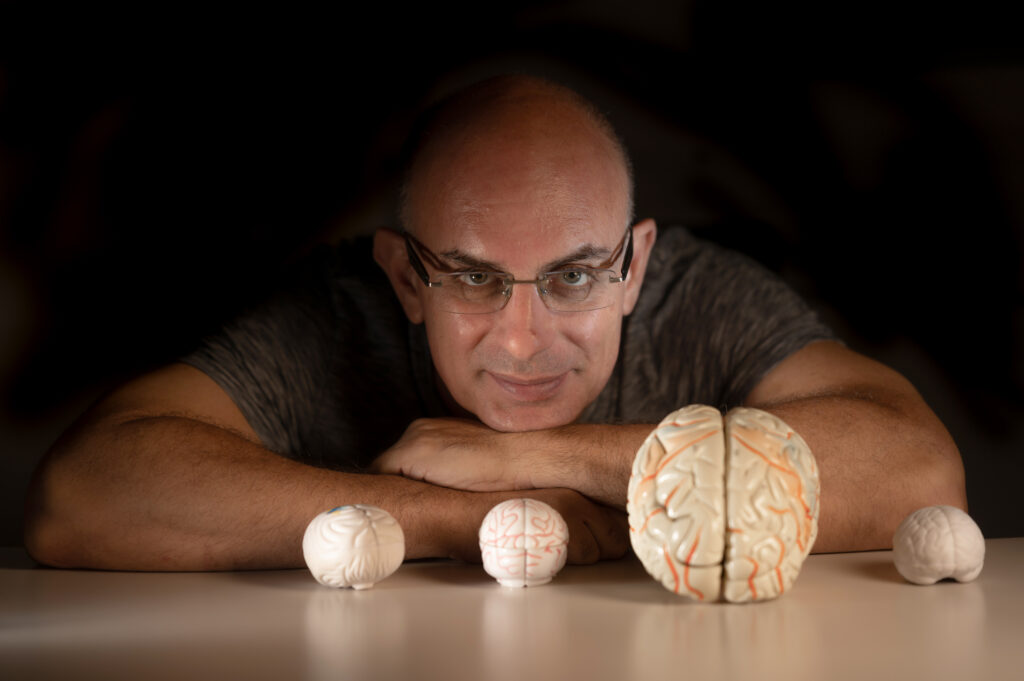
Dr. Tomer Hertz, a computational immunologist from BGU’s Shraga Segal Department of Microbiology, Immunology and Genetics, is pursuing a batch testing strategy to dramatically increase diagnostic capacity.
“The approach is trying to do more with the same number of tests,” says Dr. Hertz.
By pooling samples from many people into a few groups and evaluating pools rather than individuals, the scientists think they can use fewer tests on more people.
This approach could lead to the faster detection of individuals who are unwitting carriers of the disease and an ability to quickly clear others who have not been infected.
The strategy has been used in the past to successfully detect cases of HIV, chlamydia, malaria, and influenza, and was originally conceived during World War II to test thousands of military personnel for syphilis.
Dr. Hertz and his colleagues have developed a unique group testing method that eliminates the need to test any sample twice.
Rather than separating samples into distinct pools, they divide each sample among pools that overlap. For example, say you are testing those same 100 samples from before, one of which is positive. You then distribute those 100 samples, in various combinations, into 14 groups of 50. Each sample appears in six or seven different pools. With one positive case, a specific sequence of six pools should come up positive.
By knowing which sample uniquely belongs to all six pools — for instance, patient 74 is the only one that appeared in pools 1, 2, 7, 9, 12, and 13 — you can trace that positive result back to an exact individual without having to retest any samples. When there is more than one positive case in the mix, it gets more complicated, so the researchers designed a computer algorithm to identify all the carriers.
The biggest limitation of the batch approach has less to do with the test itself and more with the nature of the disease.
Group testing works well as long as the prevalence of a pathogen remains low. But if there are too many positive cases in the tested specimens, most of the pools will come up positive and will have to be followed up with individual tests anyway.
Dr. Hertz’s combinatorial approach works best when the prevalence of the disease in a community is no higher than five percent, with around one percent being ideal.
This is what makes this approach most effective identifying and clearing asymptomatic carriers, an essential factor in being able to reopen society.